🧠💬 Ever feel like your gut and mind are out of sync?
If you’re a woman over 40 navigating perimenopause or menopause, this episode is a must-listen. We’re diving into the powerful connection between your gut and brain—and how your gut health can influence your thoughts, mood, and even how you advocate for yourself in medical care.
In this enlightening conversation, I’m joined by Dr. Cecily Havert, a compassionate family medicine physician and Clinical Assistant Professor at Georgetown University. She’s a Minneapolis native, a University of Wisconsin-Madison grad, and now practicing in Virginia. (Psst—her name is pronounced Ses-a-lee Have-ERT!)
We explore how the healthcare system often pushes both patients and doctors into burnout—and how new approaches like contemplative medicine, concierge care, and self-advocacy are shifting the landscape.
Dr. Krause’s Protocols
Instructions Included
Traveling soon? Looking to detox or reset your gut? Try one of Dr. Krause’s Fullscript plans.
✨ You’ll hear:
- How your gut-brain axis can affect anxiety, memory, and decision-making
- Why menopausal weight gain might actually be your body protecting you
- What self-advocacy looks like in a broken system—and how to get the care you deserve
- The truth about doctor burnout and how it impacts YOU as a patient
- How contemplative medicine is healing both doctors and the people they serve
- The power of building primary care offices that address both physical and mental health
Dr. Havert recently completed a fellowship in Contemplative Medicine at the New York Zen Center, deepening her ability to connect spiritually and compassionately with her patients. She’s also a writer, mentor, and co-host of the Living Breathing Medicine podcast.
This conversation is heartfelt, grounded, and full of tools for women who want to feel heard and heal better—inside and out.
👉 Listen now and take the first step toward becoming your own health advocate.
✨ Don’t forget to like, comment, and subscribe for more episodes that empower women over 40 to thrive.
🔗 Resources & Mentions:
- Dr. Cecily Havert: https://www.nvafamilypractice.com/our-team/cecily-havert-md/
- Awakened Medicine on Psychology Today: Read Here
- The New York Zen Center – Contemplative Medicine Fellowship: https://zencare.org
- Living Breathing Medicine Podcast: Listen Here
Our Partners
Podcast Transcript
Chapters
00:00 Introduction to the Health Fix Podcast
02:30 Meet Dr. Cecily Havert: A New Approach to Medicine
05:28 The Reality of Burnout in Healthcare
09:27 Transitioning to Concierge Medicine
12:11 Understanding Contemplative Medicine
19:20 Mental Health and Its Impact on Physical Health
20:40 Coping with Stress and Anxiety
24:38 Embracing the Changes of Aging
28:36 The Role of Hormones in Women’s Health
30:40 Navigating Health Information in the Digital Age
34:56 Building a Relationship with Your Healthcare Provider
39:01 The Gut-Brain Connection and Its Implications
48:26 Lessons from the Past and Energetics in Health
JANNINE (00:01.292)
Welcome to the Health Fix Podcast, where health junkies get their weekly fix of tips, tools, and techniques to have limitless energy, sharp minds, and fit physiques for life.
Hey, health junkies, on this episode of the Health Fix Podcast, I’m interviewing Dr. Cecily Havert. She’s a Minneapolis native. She went to University of Wisconsin, Madison, and now she’s living in Virginia, and she is serving as the clinical assistant professor of family medicine at Georgetown University. She mentors future medical students in the ambulatory care setting. She hosts regularly.
The North Virginia Family practices monthly town hall series and contributes to both the mindful medicine corner in the NVFP newsletter as well as her column in psychology today known as awakened medicine. Now she and I get deep into talking about how important it is for doctors to take care of themselves and when doctors
and patients are both in a rough place facing burnout, what the heck do we do? Well, it’s all about self-advocacy. We definitely talk about that. We talk about something called contemplative medicine, which Dr. Hayward is well versed in and actually completed a fellowship at the New York Zen Center just to study that in particular. Her approach to medicine is much different than a lot of
conventional docs who are still stuck, let’s say in the system. She is running a concierge care facility and still takes insurance, but she’s got it figured out and how to do it and she’ll explain it in the podcast. But really what we talk about today is really thinking about what’s going on with healthcare in terms of how we can get the best care, but also talking about our mental health.
JANNINE (02:02.666)
and how that relates to our physical health and how important it is to find a doctor who listens to you. Now, I may be speaking to the choir here, but this podcast is just a really great conversation about how key it is to think about the type of care you’re getting right now and is it serving you. So if you’re feeling frustrated about your healthcare situation,
you’re wondering what to do to find a doc who will listen and truly take care of you, this podcast is for you. So let’s introduce you to Dr. Cecily Havert. Hey, health junkies, welcome to the Health Fix Podcast. I have Dr. Cecily Havert on today and I am excited to talk about the landscape of primary medicine and how we can make it work better for all of you all and for us at the same time. So Dr. Havert, welcome to the Health Fix Podcast.
Thank you so much. I really appreciate you inviting me here.
Hey, my pleasure. I of course always connect when I see that someone is from the Midwest because there’s just something about it. Like you said, we are roots. We hold them deep and coming from Minneapolis, I’m definitely like, okay. And going to Wisconsin, you know, Wisconsin, I’m just like, this is, this is very, very connected to, my homeland. But now you’re in Virginia and doing some amazing things. And so one of the things I typically like to start my podcast off with is, is asking
Hey, what was it about being a doctor that led you to the profession? What got you here?
Dr. Havert (03:37.848)
What got me here? Being a doctor is not something I necessarily thought I would be doing when I was younger. mean, even through grade school, high school, I was actually really, really interested in the humanities. I wanted to be a writer, a journalist. And I was just really interested in the human experience. But I also really love science. I’m kind of like a science fiction nerd. I love science. And I love genetics.
everything that goes along with it. it kind of, in college I sort of had this parallel track where I was doing a lot of science courses, you know, like who takes organic chemistry for fun? You know, that was me, you know, but so I just, and then I sort of realized that, you know, I really love science, but like how can I really, you know, combine humanity and science together? And then medicine just seemed to make sense to me. And so I did a quick pivot when I was a junior in college. And I mean, luckily I’d taken a lot of the prerequisites and it just, just, it just makes
since then. So that’s kind of how I found my way into medicine and I guess you know it’s been 20-25 years now so still here.
It’s wild. I love to hear the stories because a lot of people will say it either seems like I’ve known all along or it’s like I kind of just ended up here because I’m… Yeah.
I stumbled into it, yeah.
JANNINE (04:58.462)
Absolutely can’t agree with that and you know think a lot happens in our minds in terms of that heart, those just open natured hearts where we’re like I really want to help people and this is where you know I become conflicted between the medical, the conventional medical space, the alternative medicine space, the functional medicine space, you know. We all want to help folks but at some point we all come, you I don’t say all of us but I would say a lot of us come to this point
where like, am I even helping anyone? What am I even doing here? And I’ve noticed that through your work, you’re really helping bridge that gap, but helping to find this balance between primary care and helping clients get what they truly need and what feels good for you. So tell us a little bit about how that kind of came up for you when you were like, this is not what I signed up for or not what I was envisioning.
It’s really sad, what you’re saying about, I guess we call it burnout, healthcare burnout, it’s definitely something that’s been around for a while and I think it’s getting worse. It’s something that, when you start medicine and you have these almost zealous ideals about helping people and humanity and just healing, these really beautiful goals that you want to set, and then you kind of get thrown into a system
doesn’t necessarily help you reach those goals in a way and in some ways punishes you, in other ways. It’s natural to start to feel unhappy, the joy is gone, you start to experience that burnout. so, yeah, I I went through medical school, started residency. Residency was hard. Let me tell you, I’m a family medicine doctor and I do mostly primary care of the emphasis on women’s health these days.
But residency was tough. I mean you were taught that Going without sleep going without eating this is how you need to do it And if you don’t do it this way somehow you’re a bad doctor right so it’s basic It’s really interesting in medicine. You know we’re there to heal, but how they we train our young doctors is anything but Nurturing and it has it there’s there’s really no compassion in it at all And so it’s you know so then you start to develop these ideals like I need to sacrifice everything
Dr. Havert (07:24.816)
in order to be an effective doctor. So you kind of start that mindset. then, so I got, somehow survived residency, and then jumped into the primary care realm, and I was practicing traditional medicine for probably about, let’s see, 2000, I don’t know, maybe about 15 years? 15 years of practicing? And every year, you know, just seeing, you know, sometimes 20, 25 patients a day, you know.
being rewarded only with how productive you can be and how much money the system that you can bring in for the system and really seem to take away what you know the reason why I really went into medicine in the first place. So I made a switch to go over to a particular practice of medicine called concierge medicine about five years ago. Actually almost six years ago now.
And what we do in this practice is we continue to take insurance. However, I limit the number of patients that I take on my panel. So instead of the 3,000 patients that I had that I was taking care of before, now I have about 450 patients. And I’ve capped my panel, so I don’t take any more. And it allows me to spend more time with the patients to get to know each and every one of them, and just to sort of give them a higher level of care.
So there’s a membership fee that they pay yearly, but we charge insurance. basically it’s just that extra membership fee sort of pays the overhead to make it so that I only have to see 10 patients a day instead of 25. So I really feel that the quality of care that I’m giving is higher, but then that also makes me feel the extra compassion and the extra time I have for myself. I’m actually showing myself some self-care by doing this.
it brings some joy back. So that’s one way I’m the burnout piece.
JANNINE (09:27.662)
It’s what you said at the beginning, you know what you’re doing is awesome. I think a lot of folks are are headed that way I chose sedation insurance all together and and yeah I I’ve been limiting my practice to write around 400 people a year because yeah when you get numbers higher than that it’s just it’s very hard and I think a lot of From the patient perspective a lot of patients are like well, you know, the doctor doesn’t care They don’t you know, they don’t take me
personally, right? They don’t invest in me. And the truth is, like a lot of us just in the practices where it’s money driven, you know, the big practices, it’s not that it’s that, you know, like you said, the bigger producers, the more people you can see in the amount of time. And at the end of the day, I was trying to do that during COVID in particular when everything was really kind of haywire and it just didn’t work. And I think for a lot of doctors, know, and this may be happened to you too, you get to this point where
Yes, the training at the beginning and we didn’t have residencies per se, we kind of did them while we were in school. But you get it stuck in your head, like you feel guilty for taking a vacation. Correct. I don’t know if this happened to you.
No, no, no, absolutely. yeah, you feel bad. It’s just, know, and that’s why so many healthcare providers and practitioners work over our vacations. I mean, it’s taken me, I mean, I would say that probably I still kind of do it, but it’s taken me a while to really be like, to try to disconnect because you just, feel guilty if you aren’t, you feel like you’re letting your patients down. And then you start to develop this narrative in your head of I’m a bad doctor if I don’t do this, right?
piece really starts to eat away at that. And so that’s what I’ve sort of recognized as as some of my biggest demons and how I’m really trying to turn things around.
JANNINE (11:22.254)
100%. Yeah, this is a big, big issue I see for sure too. With myself, it’s, know, can I completely disconnect? Not yet.
No, no, you know, and there’s, yeah, there’s something, yeah, that, that, yeah, we just feel like we’re gonna let somebody down if we, if we completely disconnect with it.
Absolutely, absolutely. So of course, you know, this is kind of the doctor perspective I like to bring that in a little bit so folks can see this side and then there’s the side of of patients and and one of the biggest things that you focus on is is mental health aspect of things and This is where I see Needing more time with people right needing more time with the behavioral health things of that nature and and you You’re you’re you’ve taken extra training in contemplative medicine I think a lot of people don’t know what contemplative medicine is
Please, please let us know about that. Tell us what that means and how that helps the mental health side of things.
wow, I mean it helps every side of things. about a year ago, a year and a half ago, I participated in a year-long fellowship in contemplative medicine. And this is a program that was founded by the New York Zen Center, which is a Buddhist Zen center right in the middle of Manhattan, which isn’t a very Zen place as far as most people think. I mean it’s like on 23rd Street right in Chelsea.
Dr. Havert (12:47.344)
What I love about it is you’re just able to be in that space but still find your inner sanctuary, your inner peace. But anyway, there was about 35 of us. It was a cohort of healthcare providers and doctors, nurse practitioners, PAs. I think those were the main people that were in there. But all specialties. had orthopedic surgeons. had psychiatrists, a lot of palliative care doctors. But we all came together.
and it was a year-long fellowship in sort of just understanding, looking through the lens of Buddhism and infusing more compassion in how we go about healthcare, both in how we treat our patients, trying to create a more compassionate space for them, but also create a more compassionate space for ourselves. Because honestly, know, what I found…
most compelling when I first started the fellowship. went in there thinking, I’m going to do this for my patients. I’m doing this because I want to be a better doctor for them and this and that and everything. then so much of that after the first few months, I started realizing that so much of the work was you’re really turning the lens inward. And you can’t really be that for somebody until you’ve really found that space for yourself. And so that was hard because it’s a lot easier to try to fix other people than to try
fix yourself. in some ways I mean but
So that was the big piece and it just really helped me find my vulnerability, my ability to, this is what I kind of always go to, these are some of the biggest sort of ideas that came out of this was the pause. So before you go in and you see a patient just really just taking a moment to kind of clear your mind and just pausing, taking a minute to yourself, whether it’s you’re washing your hands or just a couple of deep breaths and that really allows you to ground yourself.
Dr. Havert (14:52.244)
going in with the then the second one is going in with the beginner’s really so like no preconceived ideas about how you’re going to treat this patient if you’ve seen this patient before and you know and if it’s a challenging case or you know you know just so you don’t know preconceived ideas just go in there with the beginner’s mind and then the third is just bearing witness and that’s just really just sitting down and completely allowing the patient or the client just to talk and just you just listen and you take it in
and you don’t try to fix, and you don’t try to, you know, I mean, obviously they’re there because they want something, but a lot of what people, what I found that patients really need is somebody to listen to them. And so a lot of what we were doing was this sort of this act of really active caring listening. And then when people feel held and safe, then you can start to get to work.
So that’s sort of, I mean, it’s sort of a mouthful and we did a lot of other things in the fellowship as well, but it really just sort of changed the way that I approach how I go into a patient care setting, both for the patient and myself.
It’s definitely something that I think holding space is probably the most healing of anything we can do, even though we’ve been taught to like think through algorithms, think through, you know, would this work better with that? But I found like, like what you’re saying, if I can slow down and just sit and listen and not have it rolling through my head, I’m going to do this. that’s going to work. maybe I should try this. It’s to unfold by the end magically somehow, I’m guessing.
It really does. And it’s not to say that that stuff isn’t sort of happening in your head, because I mean, you are conditioned a little bit, you know, to try to figure out about that piece. But like you said, it’ll come out in the end. And it’s really about creating that interface with you and the patient. And just developing that layer of trust.
Dr. Havert (16:55.22)
You know, the other thing that I found stressful about being a healthcare provider is that sometimes you’ll see really, really challenging patients that the presentation doesn’t make sense or maybe they’ve been to lots of different providers and they have lots of symptoms that don’t make sense and you sit there and you listen and it doesn’t make sense to you either. And then instead of, a lot of what we’ll do is we’ll sort of project our frustration of not being able to figure things out on the patient.
And so just sort of noticing our own fear of failure, of not being able to meet the needs of a patient. It was just sort of noticing that.
That would be something that would sometimes come instead but just really sort of that beginner’s mind and bearing witness and really listening to the patient and just Even repeating back what they’re saying and just saying that I’m willing to go on this journey with you I may not know exactly what what’s going on right now, but I’m willing to be curious and let’s start this together Sometimes that’s all they need and you almost diffuse like their defenses that come in also so
Yeah, it’s wild how we feel like we have to have an answer. We have to have a solution. We have to have something. And like you said, sometimes it’s just like, I’m going to come on this journey and we’re going to figure it out together. think in probably the last couple of months, I’ve really come to really embrace that because people are getting sicker and there’s more complex things going on for sure. And I’m sure you’ve seen that as well.
Yeah, well and then you also have to recognize the interface between physical health and mental health and there really is no way to separate the two. And so that’s the other piece of it is sort of there’s always a mental health piece. mean even if you’re patient coming in with a cancer diagnosis with lots of physical symptoms, how can that not impact your mental health? And so really trying to address that and then understanding how they interact.
Dr. Havert (18:59.054)
interact and affect one another and allowing patients to sort of, you know, be curious about it. You know, it’s just, sometimes it’s not something that people completely want to be open to right away, but it’s something that I think is really important and eventually you can hopefully get there with most people.
It takes time, right? It takes time and takes some patience and definitely, yes, this podcast is not necessarily practitioners, but I think it’s really great for folks to hear our side, but also kind of think about like, okay, it’s a relationship. I’m, anyone who’s doing a membership program or concierge type of program, you’re in it for the long haul with us. It’s not a one and done, you know? And so thinking about how you can develop that relationship. One of the things we chatted about before we even hit record and just
little bit ago is how a lot of folks are struggling mentally right now because there’s a lot of change in the environments, know, with jobs and government stuff and elections and whatnot. And while I don’t…
particularly talk about politics ever, it’s not my jam. I’m more interested in someone’s mental health. I’m more interested in how their thought process affects their health and how it carries into like all of their habits, behaviors, routines. And one of the biggest things I’ve seen with a lot of women lately is that we’ve got a whole issue of stress eating around what’s going on. And then you pair that with hormones declining and estrogen in particular driving to eat more carbs. And so it’s this thing. So.
What kind of tactics do you have for your clients to help them when their minds are kind of pinging on all of these things that they can’t necessarily control?
Dr. Havert (20:40.238)
Yeah, I mean that’s tough. mean that’s the crux. That’s what we all need to figure out, right? I mean, I think, and I agree. I right now I work outside of Washington, D.C. And let me tell you, there’s a lot of stress, there’s a lot of really, there’s a lot of heaviness, there’s a lot of uncertainty. Uncertainty plus fear equals anxiety. So I tell my patients a lot of right now, both of those two factors are really high right now. So yeah, I mean,
you know, part of it is just,
Obviously there’s a few coping mechanisms, things that we shouldn’t do. I doom scrolling, constantly turning on the news, and just engaging over and over in the narratives, whatever narratives they are. That’s not necessarily a helpful thing. mean there’s a lot of, what that does is it kind of pushes us into the state of survival, hypervigilance. We’re really just trying to protect our well-being, and so that really
gets our defenses going, right? And so that doesn’t necessarily feel good for our body. That affects our sleep. can affect our, it makes our muscles tight. mean, we just, you know, it can affect our gut. There’s a big connection between our mind and our gut. So I think probably the first step is just noticing, is just noticing the impact that this line of thinking and these maybe unhealthy coping mechanisms are having on our body. So there’s that piece trying to remove some of those, you know, that doom scrolling.
peace can be really can be part of it. If you’re really struggling with your sleep, know, you know, lots of ruminating thoughts, worry, you know, definitely reach out to a health care provider. I mean, if you have a primary care doctor, that’s a really great place to start. Most for most people, you know, we I kind of see us as sort of the interface between the physical and the mental health and we can help navigate some of that space a little bit. Finding a therapist, somebody to talk to can
Dr. Havert (22:43.82)
really, really helpful. there’s, so you we want to support that piece of it. But other things that we can do, you know, that, that, you know, and I do work with a lot of women, especially a lot of women in sort of the perimenopausal, you know, stage of their life, which I know a lot of your listeners are, so we can, we can speak to that. But I mean, it’s not an easy time to begin with, right? And then you add extra stress on top of it. And you know, that’s, it’s, not always a pretty thing. But one of
the
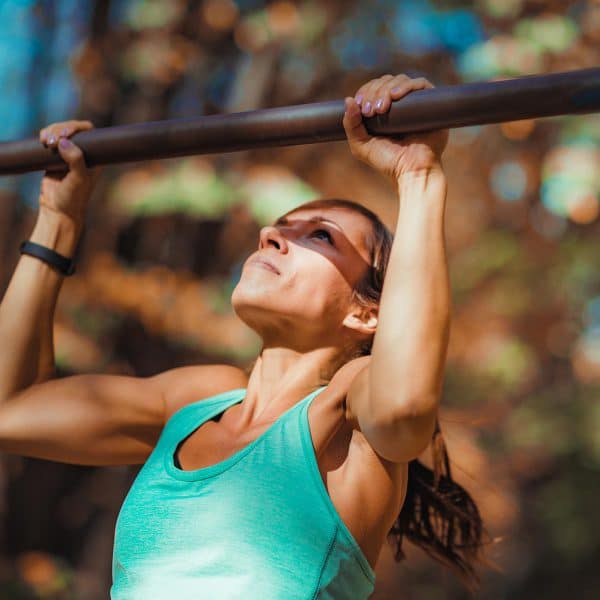
The treatments, I guess, if you want to put it that way, that I’ve really been trying to encourage people to be curious about and maybe try to adopt a little bit is exercise and moving your body. say strong is the new thin, especially for us, know, paramenopausal menopausal women who are having lots of changes happening in our body, which physiologically actually should be happening. You know, I mean, there’s a lot of changes happening with our hormones and there’s going to be, our bodies are not going to look the way
they did in our 20s, nor are they supposed to. So exercise, empowerment, really starting to love ourselves and love our bodies is one way to really try to kind of elevate ourselves outside of a lot of the other stressors. Just gaining control and feeling good about ourselves is one of the big things.
You mentioned something that I don’t think I’ve highlighted on enough in the podcast is really that our bodies are naturally meant to change. And if we look at social media, we’re scrolling, we’re seeing like people say, get back to your, you know, you’re, you know, look like you’re a 20 again, things of that nature or feel like you’re 20 again. And I’m like, wait a minute, physiologically we’re meant to change for a reason. Can you speak a little bit more to, to the body’s changes? I haven’t talked a lot about, you know, what’s supposed
JANNINE (24:38.274)
to happen first thing, you know, technically what physiologically is supposed to happen or what may be protective for us. I think that might even be a better word because a lot of women aren’t thinking about like why would we end up shifting our hormones? How can this protect us? How can a little, you know, of these things help us?
Yeah, no absolutely. Yeah. No, I mean during I mean our hormones change all through our life. I mean just think puberty Whoo, you know like talk about hormones. Okay, what’s happening during puberty is our hormones are are are actually Going up very very quickly and there’s a lot of changes that occur during that and I’ll just mention that in medical school We spend a you know, we spend this fair amount of time talking about the health of young women right going through menopause reproductive age You know OB GYN,
We spend a lot of focus on that. I don’t have to say, I have to admit, and maybe things have changed since I’ve been in medical school, but we didn’t spend a whole lot of time talking about menopause. It was sort of like just something that, oh, you know, and to me, like, oh, that just sort of happens, sweep it under the rug. And it made us feel like it wasn’t important or maybe even something to be ashamed of. So it was really, it was interesting because when you have doctors and healthcare providers that are, you know, getting those messages even subliminally in their education,
And I think it’s a commentary of sort of how society necessarily has felt about aging women. But anyway, that’s just sort of my side, my side little sidebar there. But as far as what’s actually happening in menopause is, like I said, for puberty hormones go up.
things change, they go up and down during our reproductive age, ages, you if we choose to have children, pregnancy can affect those as well. Menopause is basically when these hormone levels start to drop. So we see major drops in our estrogen and our testosterone. Those are kind of the main, and our progesterone somewhat, but estrogen and testosterone are the big hormones that really start to drop during perimenopause. So that would be, you know, around maybe, well, for every woman it’s different, but we’re gonna say between 45 and 55.
Dr. Havert (26:48.096)
of these changes are occurring. you’re gonna feel it. mean, it’s not, some women are, everybody has their own experience with it, but what can happen with that drop in estrogen is hot flashes, you we probably hear a lot about that. So the vasomotor symptoms, so the hot flashes, poor sleep. What also starts to happen is our body composition starts to change. Okay, like you said, physiologically, this is happening because our estrogen levels are
falling, right? So when our estrogen levels fall, what starts to happen is we also start to lose some lean body mass, some of our muscle mass, and the fat mass starts to go up a little bit, okay? And so when our estrogen levels fall, it’s because our ovaries are not producing as much, but we still need some estrogen. So a great source of estrogen in our body, believe it or not, is adipose tissue, is fat. We’ve got hormones,
or enzymes that convert adipose tissue to estrogen. So our body is saying, estrogen’s going away. Well, I’ve got a solution for that. Let’s just put on a little bit more fat mass. We’ll bring the lean body mass down. We’ll bring the fat mass up. So if you think about it, it’s sort of, I mean, it’s not what we want to happen or what society has taught us, what we’re supposed to look like. But it’s really just, it’s sort of a natural phenomenon.
So yeah, so there’s that piece of it. So that’s sort of when we see kind of the, you start to see some weight gain, especially like I usually say between like 10 and 20 pounds during menopause is actually a very common thing to occur. So that is something normally that can happen.
Yeah, and I mean, and I love that you say that because, you know, the more I look into it, because of course, you know, I’m on the side of bioidentical hormones, helping with different hormones and hormone replacement therapy. And a lot of women, I’m gonna blame TikTok. You know, we have a lot of TikTok folks saying, I put estrogen patches on and my weight dropped off. And it’s not really.
Dr. Havert (28:58.542)
No, I will say that that’s when I because I also use on hormones a fair amount to bio identical I prescribed them by identical hormones and I would women say oh well this helped me lose weight I said probably not
You’re like,
mean, there are other things that you can do in addition to, but it’s nothing magic. Hormone, especially estrogen replacement, is great for vasomotor symptoms. I see a lot of, we think that there’s probably some, like our joints, there’s probably some inflammatory changes that happen when estrogen levels drop. And so I see women actually feel a lot better with that. Their sleep is better because a of times they’re vasomotor. So those are some of the
the benefits of hormone replacement.
Absolutely. Yeah, I, you know, just like you, even in naturopath school, we talked about perimenopause and period, regulating periods and that stuff. like, boy, once it came to menopause, it was like crickets. You know, what do you do? How do you keep, how do you do the longevity thing? know, how do you do those kinds of things? It’s, it’s interesting. And so that’s why I’ve kind of dove into it because I’m like, this is where I actually, this is how I got into this. you know, my mom died of cancer when I was 26 and I was like, I’m not going out like that. You know, and I’m like, I’m, I’m
JANNINE (30:17.904)
to know how I can live to at least a hundred and I’m trying to shoot for that. And I think for a lot of women we get to this point with our healthcare where maybe we’re not finding a provider we resonate with. We’re not finding the right care and then we get confused as to what to do and so we start looking at social media. Let’s talk about that for a second.
Dr. Google comes into my exam room a lot.
Have you had Dr. Chat GPT? Because that one blew me away recently with a patient that said, I asked Chat GPT my symptoms and this is what it told me that you need to do for me. And I’m like, OK.
Yeah, no, that’s a little, yeah, that’s a little dicey. I I want everyone to be advocates for themselves and their health and everything. But the problem is that it’s hard to sift through the information that’s out there because there’s so much information, right? And if you…
And you can, if you choose to look at it through a certain lens, you will find information that will support that.
Dr. Havert (31:30.57)
lens that you’re looking through, right? I mean, that’s just sort of what it is. so, you know, and it’s, and I, what I tell people is, know, just be curious. Don’t necessarily take it for, you know, like this is, you know, I mean, I just be curious. I’m glad you’re advocating for yourself, but you know, really still trust in the healthcare system. mean, the training that we’ve had is, you know, it, it, you know, I’ve been, I’ve been practicing for almost 25 years now.
And just the experience that I have, way that, you know, CHAP GBT and Dr. Google doesn’t necessarily know your family history. It doesn’t know the, you know, the lead up to the month before or this or the mental health implications or what other things you’re dealing with, you know. And so it really doesn’t have that level to kind of piece through. So I’m like, okay, if you want to advocate for yourself, that’s great, but really be cautious and just more curious, right?
rather than this is what it is.
Well said. Well said because, you know, yes, I keep trying to tell folks, you know, it’s really, and this is all joking aside, but you’ve got folks who are not medical professionals training bots here, you know, and they may be 20-year-old folks in a computer room training a bot. So it’s very important to realize that you’re not, don’t have docs, like Google Doc isn’t really a doc trained thing in chat to GPT. I have no idea who trained it.
I
Dr. Havert (33:02.232)
I don’t know, I I’m sure that there are algorithms. There’s always an algorithm. But you know what, I don’t, like I tell my patients, I don’t treat you by, I I may use an algorithm sort of as a basis, an outline. I treat the patient, I don’t treat the labs. I don’t treat the algorithm. You know what, you are a completely individual person with your own experience and you just, really have, it’s hard to treat, teach a bot how to think outside the box.
What’s interesting, but I’ve also noticed is that these
these AI systems usually have the worst case scenario. If they’re gonna give you a differential diagnosis, the worst case scenario is always on top, and that’s the thing that we think of. But in medicine, all of those differentials are maybe in there, but we can weed out this one because I already know this about you, so this can’t possibly be true. yeah, so it is interesting, it can be terrifying.
You Google fatigue and it says that you have brain cancer. mean, of course you’re going to be scared, right?
Right, right. know, rash, night sweat, know, especially night sweat and all that, you know, it’s, incredible. So, you know, it’s one of those things where getting to know, and this is what I tell folks all the time. said, like you just said, you know, you, know, this isn’t true about you because you already talked about that. We’ve listened to you this is why I love concierge programs. Why I love consistency with the, with a patient because we know your history. We know what you’ve been
JANNINE (34:43.38)
we know what surgeries you’ve had, we know all this stuff and we’ve heard you over and over again. And this is where I really wanted to kind of wrap this and bring this all full circle is creating a…
a relationship with your doctor. I mean, I’m not saying you guys are gonna hang out and do things like that. That’s not exactly the idea. It’s more the idea of looking for someone that you align with, that you can really sit down with and talk to. So for folks that are going, know, maybe their primary, and this is happening for a lot of people, their primary care provider retired, I still go to Washington from Wisconsin because I believe so much in continuity of care.
people. just do. And so with this in mind, what kind of advice do you have folks that are looking for maybe a concierge doc or someone in their area that’s maybe doing one of the membership programs that’s like a… I can’t think of the thing…
There’s drug primary care, DPC. Yes, that’s exactly. And yeah, you know, it’s hard. Because the reason that there’s a lot more of these DPC and concierge medicine and membership practices coming up is really because the health care system, especially for primary care, doesn’t support what we are trying to do for patients. Right? I mean, you hear people complaining, like, well, my doctor doesn’t spend enough time for me. I feel like I’m just a cog in a wheel or I’m on a
conveyor belt. We recognize this and you know we were also part you know a lot of us who’ve left that system were part of it and just couldn’t do it so yeah so these these new systems are starting.
Dr. Havert (36:24.462)
But you know, they cost money, right? mean, it’s just like in our mind also we’ve used our insurance. Well, our insurance should pay for everything, but it’s like we almost have to kind of change our mindset a little bit. Like, well, how much are you willing to invest in, you know, finding someone that you can work with and that you feel safe with and that’s going to listen to you and everything. but yeah, so anyway, so there is that little piece of it that not everybody can afford, you know, these types of membership practices.
and so there still thankfully are other forms of primary care out there. But if you are interested and have the resources to do so, really when you find a membership practice like this, interview the doctor or healthcare provider and just see if this is somebody that you can work with. I you really want to be able to see if you can align, ask questions about how long
are your appointments and know, what are your wellness or your physicals like? So really trying to get to know that doctor and then that doctor or the healthcare provider should also ask you questions too. Trying to get to know you as a person. it really is all about just, I I hate to say it’s like you know like swipe left, swipe right or what is it like speed dating or anything like that but it is. It’s sort of you know if this is the type of healthcare that you’re looking
for and that is important to you and something that you’re willing to invest in, then really kind of interview it like you would a job.
Makes perfect sense. makes perfect sense. Now one of the other things that I’ve kind of told folks that who can’t afford this type of care is to look for providers that are also, they have town hall series like you have, or Q &As or podcasts. So you can gain more information. You can learn maybe what you can’t get from your primary care and really finding resources that are solid and reputable to help support your.
Dr. Havert (38:31.778)
That’s a really great point. and I’m really I mean what’s also what with this type of practice of medicine allows me to do is to really get more involved in my community and provide more education opportunities and that that’s something that that drove me to this because I really like to connect with more than just the people that are in the exam room. I just feel that there’s you know, there’s so much more that we can do outside of the walls of you know, the clinic. But yeah, no, absolutely, you know, find good. There’s so many.
good town halls out there. know, our practice does it. I’ve actually got a town hall coming up soon talking about GI psychology and the interactions between the brain and the gut. That’s next week. I’ll send you links for that if you’re interested. yeah, no, it’s sort of, know, kind of, you know, find these doctors, you know, look on their websites. A lot of times we have a lot of extra, you know, podcast resources. So you can maybe learn something and feel
and feel supported and connected.
Absolutely, absolutely. you did drop the green, the, I can’t green, well there’s that, grains. My gut, I think a gut and then my brain goes.
And they should, I don’t know, honestly.
JANNINE (39:46.926)
It’s so funny, Freudian slips are hilarious. But yeah, the gut brain acts as a lot of people are, you know, it’s been around, we’ve talked about it for a while, but a lot of folks are really now just coming to it again, maybe, and really starting to realize how much what you eat has an impact on how you think and how your brain and nervous system work.
So could you tee us up a little bit for your presentation? Give us maybe a little bit of background. So folks who have maybe never really thought about gut brain access or they’ve heard about it, but they would love to hear your take on it. Could you give us a little bit?
Yeah, sure.
Well, I mean, yeah, no, I agree with what you’re saying. I think that nutrition and what we eat and how our food is prepared, I this is tip of the iceberg stuff, right? I mean, we’re still learning all about that. This particular town hall, I’m bringing on Dr. Ali Navidi, who is the founder of GI Psychology. And so he’s a psychologist who offers basically cognitive behavior therapy and hypnosis for patients who have irritable bowel or
Oh yeah, who have functional gut issues. A lot of times related to stress, anxiety, depression, a lot of times they go together. But it is sort of using the brain as a kind of a conduit for healing. And there is a lot of data, good data, that shows that using these types of strategies can be really helpful for treating and even curing functional GI distress.
Dr. Havert (41:23.514)
So that’s really what we’re gonna be, what we’re really gonna be focusing on. know, IBS, irritable bowel, you know, what is that? I mean, obviously, like referring to, you know, different food, nutrition. I mean, again, we’re still learning so, so much. So that’s also part of it, but we’re really focusing on how we can use our mind and, you know, mindfulness, cognitive behavior therapy, and hypnosis as ways to sort of connect and heal the gut.
the other side. okay. Even even I mean, even more intriguing to me because it’s one of those things, right? Where and you’ve probably seen this in your practice. You’ve tried all the nutrition things you’ve tried all the diets, you have people who have done every SIBO test and every SIBO diet.
every FODMAP diet variation that they can possibly find, It still can get bloated. Yeah.
Yep, and they still book. And so in this case, you know, just for folks who are listening that are like, hmm, okay, brain, like a lot of people say to me, Joe Dispenza stuff. and, you know, Joe Dispenza definitely pioneered in this department, but, also looking at how we take, mean, let’s put it this way, a lot of women
especially by the time they get to this age, especially if there’s SIBO on board or chronic bloating, we’ve now deemed food the enemy. And so now this is its own stressor in and of itself.
JANNINE (42:48.608)
and coming in on the nervous system. How do you work right now? We’ll tease people about going into the town hall, but for now, how are you working with the brain in your office with folks? What are you teaching and how are you helping folks get out of their food mindset to control things and getting into how the brain can help with the gut?
Yeah, well, so I’m not a psychologist or anything, but what I like to do is I like to bring curiosity around it and just sort of like introduce it because a lot of times like Having it when you when you bring up to some people’s like they’re coming in there There are a lot of distress and if you tell them oh, that’s all in your head I mean that it’s not what I’m saying, but but you know then they’re just then they think you’re dismissing You know it’s like what do you mean? I was like clearly I’m having symptoms. It’s like my brain is not you know so this allowing them to be
curious about and starting to understand the connection between the mind and the gut and actually just the rest of our body. I mean our body is just a you know I try to also teach what symptoms a lot of times in the body is just your body’s way of trying to communicate with you right and if you know and if we are
you know, a state of trauma or in a state of panic and worry, our bodies, our messages are also going to get.
going to get louder in a way. so, know, it’s really, and just sort of, I think just sort of noticing the, you know, the ebb and the flow of our symptoms and where our brain is at that time. And just sort of like trying to just redefine the relationship that we have with our body and not necessarily to always be scared of a symptom, to maybe be more curious about it. Like, well, what else could this mean? And so really that that’s really what I try to do for patients is just, you know, try to get
Dr. Havert (44:40.688)
them to at least be open to that. I mean, how many times when you’re nervous and you’re gonna give a talk, you feel butterflies in your stomach, right? I mean, that’s actually your body communicating to you. It’s like your brain is worried, your body, that’s where your body feels it. So, sort of like, well, how does your body feel in that moment? well, have butterflies in my stomach, I butterflies in my chest, okay. Your body’s communicating with you.
And sometimes just recognizing that, all of a sudden it’s like, well I don’t have to be scared of that. Okay. Alright.
That’s huge because I think a lot of people will feel that and then they’re like, no, no, I’m gonna have another episode or no, this isn’t gonna happen. And then it just potentiates, I feel like it just goes down that downward spiral from there.
Yeah, so a lot of grounding, a lot of trying to find a person’s window of tolerance of being able to hold uncomfortable feelings and fears, but still feel regulated and have compassion for it rather than fear. And so there’s training in trying to get people to that. And that’s also where the more I know patients, the more trust they have in me, the more time I spend listening to them and bearing witness to what they are.
safe enough to do that and then you actually see their symptoms get better, you see them start to relax. I it really is a beautiful thing when you can kind of connect and ground a patient.
JANNINE (46:11.892)
Absolutely, absolutely. And you’re doing that. That’s really cool. I have not heard as many people working on that directly in inpatient visits. I know sometimes, you know, we will get deep into investigating and whatnot and and then send the patient home with a quick demo. But you are it sounds like you are actually doing it.
Yeah, it’s a process. It’s not to say because I am also doing the medical workup piece, right? It’s not like I’m saying, you know, I tell patients I’m like, you know, this is what we’re gonna rule out And once we rule it out, we’re gonna be curious about these other things if we rule it out So, I mean there there is that process but it’s you know It is a process and just getting people to understand and trust and trust in trust in you but also trust in their own bodies because I think a lot of people come to me and they really they they fear there’s health anxiety they fear
what their body is doing, they fear for their mortality. Yeah, it’s something that I really try to kind of create a safe space to process.
I think the fear is real. So it’s so ingrained. We have that question on our intake. What are you most fearful about your health? And it’s the most fascinating question for me to read on every single intake.
Yeah, and that’s a lot of times what you know a lot of times when I’m seeing a patient and you know They’re they’re explaining all of these symptoms and this and that and maybe they’ve seen a few other doctors before you You know, I’ll listen to all of it. I’m like, okay, this is what you’re saying I’m like and what are you afraid of?
Dr. Havert (47:41.134)
What are you most afraid of right now? Because sometimes if they say, well, I think that it’s this, and I say, well, I can tell you right now that I don’t think that’s what it is. We’re going to continue working. And sometimes it diffuses once they get it out. Once it’s out in the open, you’re like, oh, OK. Well, let’s work with that. Let’s work with that first and foremost.
Absolutely, absolutely. such powerful stuff. Now, I have been trying to read what it says behind you in terms of your picture that you have on the top. And so I would love to round out the podcast fully with what it says behind you because I see the past, present, future, and I know that there’s probably some wisdom in there. Can you read that?
Of course, there’s a couple of signs. The sign on the top says, past is your lesson, the present is your gift, and the future is your motivation. So that’s that. then the bottom, they also have a sign that says, a little bit more humorous, please take responsibility for the energy you bring into this space.
Mm-hmm. It’s…
At the end of the day, do you believe it is energetics? There’s a lot of energetics involved here where energetic means and bringing how we show up in addition to how our clients show up, there’s gonna be some interaction of our energies and definitely when it comes down to chronic health issues or it comes down to not feeling like you’ve gotten to the bottom of something, this is where energy does.
Dr. Havert (49:22.983)
I agree.
such good stuff. So, Susley, we gotta tell everybody where they can find you in Virginia, how they can get into the town halls no matter what.
Yeah, we have them every month.
I’m not sure when this is going to air, know, it may have already passed, there’ll be a link to that that podcast or the town hall on our website. But so I practice at Northern Virginia Family Practice and I we have two offices, one in Washington, D.C., one in Arlington, Virginia, and I work in the Arlington, Virginia office website NVA family practice dot com. So and as a Nancy, he is in
V is in Victor, A is in Apple, FamilyPractice.com. And if you go there, then you can, we have all of our kind of media things. can click on me and if you want to any of my posts in Psychology Today or see any of the town halls or other podcasts I’ve done, you can find that.
JANNINE (50:25.838)
Awesome, awesome. It’s great supportive information. That’s why I do this podcast to help support what I can do in the office and it really is great to have folks like you come on and share your experience and I’m really excited about this this Gut Psychology one and oddly enough I’ve caught up my podcast. this comes out next week so folks will really hear.
Yeah, it was really great talking with you. Thank you so much for allowing me the time and the space to talk about these important topics.
My pleasure, my pleasure. look forward to sharing this one. Hey fellow health junkie, thanks for listening to the Health Fix Podcast. If you enjoyed tuning in, please help support me to get the word out about the podcast. Subscribe, rate and review and just get that word out. Thanks again for listening.